Currently, the Australian Government National Security division assesses the National Terrorism Threat Level as Probable (Australian Government 2018). Further quoting from that reference “credible intelligence, assessed by our security agencies indicates that individuals or groups have developed both the intent and capability to conduct a terrorist attack in Australia”. The advice goes on to suggest that a large, coordinated attack is considered possible and that explosives and firearms are likely weapons of choice for such an attack (Australian Government 2015).
Given that we are probably going to have further terrorist attacks, and possibly on a large-scale; my question to the audience is: are we medically ready for a mass-casualty terrorist event in Australia?
Whilst on face-value, most people reading will likely think that our emergency services will cope quite well with such an incident, and I tend to agree, I would like to use a few case studies from my past to try and paint a more vivid picture of exactly what we can expect on the day, in order to get people thinking harder on the topic. Having had the rather unique opportunity to medically treat blast and high-velocity gunshot injuries at many levels of care, from point of injury, through evacuation from the field, resuscitation in the Emergency Department, and on to initial wound surgery, I hope that my opinion might add value to any dialogue on the topic, and stimulate debate about how we might better prepare for a domestic mass-casualty terrorist incident in Australia.
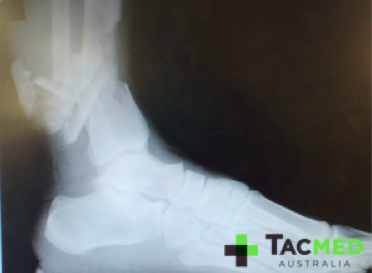
I would like to start with a single case study from my time with the Army and build from there. For anyone who has read my previous article titled why I’d rather be shot with an AK47 than an M4, you’ll be familiar with these first few images. If you haven’t read that article and want to you can find it linked here. I’ve chosen to start with this case study to get the audience thinking about how many resources a single high-velocity gunshot wound to a single casualty would tie up were it to occur on the streets of a city near you. In this hypothetical situation, let’s assume that there were Police nearby and the threat was rapidly neutralised with only the following casualty.


What then? The medical first responders in this scenario are of course the general public and the Police Officers who immediately responded to the threat. The casualty would be screaming in pain and the wound would be bucketing blood, with a very real risk of bleeding to death if not managed appropriately. Complicating the scene is likely to be confusion as to whether the shooter was acting alone, and the possibility that he may have had other weapons including explosives with him. The ambulance will have been called, but may not be in attendance with medical supplies for 5-10 minutes. If there is a concern of multiple shooters, or explosives, perhaps a cordon has now been set up and the ambulance officers aren’t coming in to the hot zone until it can be cleared. Are our Police Officers currently appropriately equipped and trained to deal with this relatively uncomplicated medical situation for the 5-10 minutes or more until the paramedics arrive?
Let’s assume that the ambulance gets there in a timely fashion and extracts the casualty. For those that work in the Emergency Departments of Australia, can you imagine the scene when this casualty arrives? At a minimum this will immediately tie up a resuscitation team of approximately six staff, the casualty will need blood which will tie up pathology staff and use up valuable supplies, he will require an emergency operating theatre organised and an anaesthetist and a surgeon or two, plus additional theatre staff to facilitate his emergency surgery.

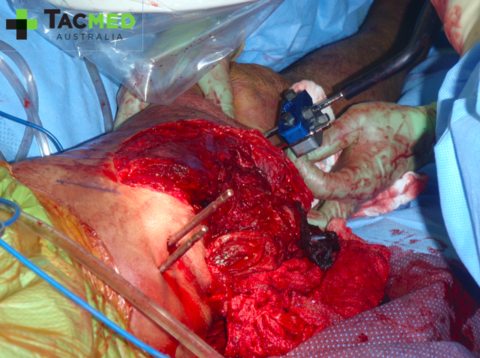
He is likely to then go to an Intensive Care or High Dependency unit post-surgery where he will require around-the-clock intensive nursing care to manage his wounds and pain relief. From there a long hospital stay would ensue with multiple subsequent surgeries and significant physical and psychological rehabilitation. All of this from a single bullet hitting a single casualty.
It can be seen that there are many critical steps in the chain of the survivability for this casualty, but the first step is always the actions of the first responder, in this scenario the Police Officers. It is widely acknowledged that the fate of the injured often lies in the hands of the first responder, and it is crucial that the early management is effective and timely in order to preserve life long enough for the casualty to reach higher care. This requires a degree of training and equipment.
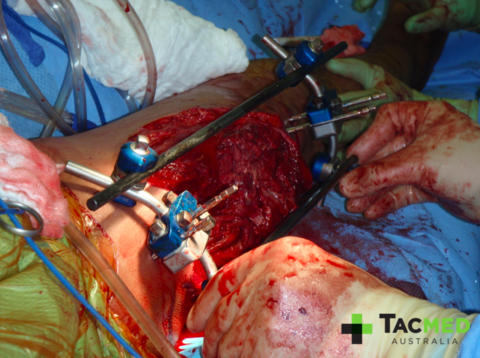
Now let’s build on the scenario and add a second casualty to the mix. Let’s say another bystander was shot through the neck in the event, and remained conscious but was rendered immediately quadriplegic by the wound.

Now the police on scene have the dilemma of a second critically injured casualty on top of the one bleeding out from his leg, and the uncertain tactical situation on the ground. All of a sudden one ambulance crew is not enough, and a second ambulance will need to attend. Having two casualties starts to introduce the concept of triage, or prioritising of the casualties, in order to treat the most critical first. It also begins to introduce the dilemma of whether both casualties go straight to the nearest hospital and run the risk of potentially overwhelming their capabilities, or does one ambulance bypass the closest hospital and head for the next appropriate facility to spread the casualties out?
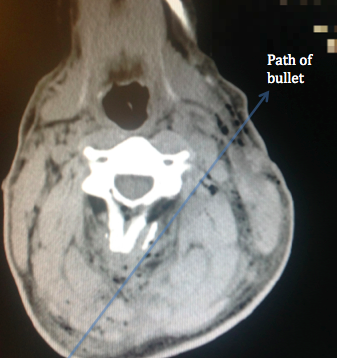
Once at the hospital, the casualty with the neck gunshot wound would receive a similar resuscitation room treatment as the leg wound, and would similarly go to the operating theatre for an exploration of his wound. He would require extensive medical imaging to assess the tract of the bullet and the damage done to his spinal cord to account for his loss of nervous system function. He too would require a lengthy hospital stay and intensive rehabilitation.
I think you get the point with the gunshot wounds, that a single bullet passing through a person can create a significant dilemma to the first-responder, followed by a massive investment of resources in the long pipeline between point of injury and definitive care. Now let’s throw an Improvised Explosive Device (IED) into the mix and see what happens. In our scenario now, the shooter has managed to inflict the gunshot wounds on the two above-mentioned casualties, and then as the Police respond, he detonates an IED which was located in a bag on the ground next to him, instantly killing himself and inflicting the following wounds on the two responding Police:


I’ve chosen to pixelate these images as to try and minimise any offence caused to the audience, however I feel that the impact of the injuries is preserved. In this setting, the casualties have minutes to live from time of injury owing to arterial bleeding from their traumatic amputations. The Golden Hour no longer applies to this casualty situation, and we begin to focus on the Platinum Ten minutes. In the scenario, even if the ambulance is nearby, given the explosion has occurred it is unlikely that the ambulance officers will be allowed onto the scene until it has been cleared of further explosives, and by that time these casualties will have almost certainly bled out and died. Of note in the photos is the presence of arterial tourniquets on all of the amputated limbs, which were applied by first-responders at the point of injury, and are the sole reason why these casualties were alive when they arrived at the medical facility where the photos were taken. During tactical medical training, not only is the rapid and effective placement of arterial tourniquets taught, but the expectation is created that casualties will apply their own if they’re able to.
So let’s take stock of the scene now. We’ve got four casualties in total, two with traumatic amputations of both legs and two with single gunshot wounds, one through the leg and one through the neck. Here we have created a mass-casualty situation which, by definition, occurs when the casualty number or severity exceeds the available medical resources available. I think the audience can begin to appreciate the complexities of all levels of medical care required to manage these four casualties. Now what if we have 14 casualties, or 40, or 140? You get the picture. There will be kids involved, there will be burns, there will be dead bodies in the streets, there will be panic.


Casualties will be peppered with shrapnel, throughout their bodies from head to toe, bones will be shattered, lungs will be destroyed by the blast.


Casualties will be pouring into the Emergency Departments of nearby hospitals by any means possible.


Does this sound unrealistic on Australian streets? I’m sure it sounded unrealistic to the residents of Boston on April 14 2013 as they finalised preparations for their annual marathon the following day, or the residents of Paris as they prepared for a night out on the afternoon of November 13 2015, or their fellow countrymen in Nice as they celebrated Bastille Day on 16 July 2016. Australia can learn significant lessons from all of these events, and the many more mass-casualty terrorist events that have come before and after them. The lessons are across the full spectrum of the medical response, but the area I will focus on is the first responder, as this is where the chain of survivability begins.
Owing to their multiple mass-casualty shootings and terrorist events, key players in the US Law Enforcement, medical and military communities convened on multiple occasions, starting in April 2013, in a forum known as the Hartford Consensus (Jacobs LM 2013). Their agenda was to translate military medical lesson-learned from the battlefields of Iraq and Afghanistan in order to optimise civilian emergency response to mass shootings and terrorist events. Amongst other outcomes was the development of the THREAT acronym (Jacobs LM 2013) for approaching such situations, which is as follows:
T = Threat suppression
H = Haemorrhage control
RE = Rapid extraction to safety
A = Assessment by medical providers
T = Transport to definitive care
Fundamental to the THREAT response is the requirement for “definitive control of life-threatening haemorrhage using tourniquets and hemostatic dressings. This must be accomplished as quickly as possible, even if the threat has not been entirely eliminated” (Jacobs 2013, p.950). No longer is the “ambulance will be right outside” approach to casualties acceptable, particularly if Australian Police are to adopt a more proactive response to Active Armed Offender Incidents.
The US have taken this response a step further in an effort to empower the general public to assist in emergency response to mass-casualty events (Jacobs 2015), with a national bleeding control campaign as part of a three-tiered immediate response to casualties (Jacobs 2015).
- Immediate responders: The individuals who are present at the scene who can immediately control bleeding with their hands and equipment that may be available
- Professional first responders: Prehospital responders at the scene who have the appropriate equipment and training
- Trauma professionals: Healthcare professionals in hospitals with all of the necessary equipment and skill to provide definitive care
The primary focus for tactical medical training recommended by the Hartford Consensus is on Police Officers, Fire and Rescue personnel, and Ambulance officers (Jacobs 2015). Despite the US having decades of contemporary military medical experience, and having had thousands of lives saved by arterial tourniquets on the battlefield, it was observed that not a single commercial arterial tourniquet was applied to one of the 17 traumatically amputated limbs, or of the other 12 severely bleeding limbs of the casualties sustained during the Boston Marathon bombing incident (King 2015). The author of the article referenced uses the phrase “lost in translation” to describe the failure of the US civilian medical sector to learn the hard-won lessons of the military. Of the improvised tourniquets applied after the Boston Marathon bombing, none were effective in controlling the life-threatening arterial bleeding (King 2015), which is consistent with the literature that suggests improvised tourniquets, even with a makeshift windlass, are likely to be ineffective (Altamirano 2015).
Whilst the French had the recent attack against Charlie Hebdo to further refine their emergency response to mass-casualty situations, it was noted that on the night of the November 13 attacks that “the demand for tourniquets was so high that the mobile teams came back without their belts” (Hirsch 2015).
Still, think this can’t happen in Australia, or that we’re as well prepared for it as we could be? Admittedly the men and women of our Intelligence Services and Law Enforcement organisations are amongst the best in the world, but the same could be argued for their French and US counterparts.
In their Active Shooter Guidelines for Places of Mass Gathering, the Australia-New Zealand Counter-Terrorism Committee cites “saving and protecting life” as the number one priority in response to an Active Shooter Event, yet it fails to elaborate on how this high priority is to be achieved (ANZCTC 2015).
Tacmed Australia and the Australian Tactical Medical Association (ATMA) feel we can do better in preparing our men and women at the coalface of Law Enforcement and emergency response to respond to a mass-casualty terrorist event. The wheel does not need to be reinvented, the hard work has been done by our counterparts in the US and around the world, all we have to do is listen and learn. The skills which need to be imparted to these men and women already exist amongst the Australian military medical fraternity who have served on recent operations around the world. Any medic who has been on the ground in the war zones of the world knows exactly how to deal with these situations because that is exactly what we were dealing with on a near-daily basis in Iraq and Afghanistan. The medical lessons-learned from the battlefields of the world translate directly to the streets of our cities when it comes to the life-saving first response to gunshot wounds and blast injuries, and they have been proven beyond doubt. Interventions such as arterial tourniquets and haemostatic dressings save lives; it’s simply a matter of appropriately equipping and training our first responders, in the Australian domestic setting being our Police, Fire and Ambulance Officers. Interestingly, these skills are as applicable in more common forms of trauma such as Motor Vehicle Accidents, as was nicely illustrated in NSW in February 2018 when a Police Officer had his life saved by the application of an arterial tourniquet to his amputated leg by a fellow quick-thinking, equipped and trained officer.
Tacmed Australia can supply both the training and equipment to prepare our first responders, however, this is not the agenda of this article. The agenda of this article is to get people thinking about the topic, to get people Googling the Hartford Consensus and Tactical Medicine, to be educating themselves and raising awareness about medical first response to a mass-casualty incident. It will not be alright on the day, and the ambulance officer may not be coming into the hot zone to help.
Australia is currently in the unique and enviable situation of being able to prepare for the event before it occurs, and not retrospectively implementing training as a knee-jerk reaction after the event, and after lives have been unnecessarily lost. The smartest minds in the country suggest that a terrorist attack is Probable at this very moment, we should Probably be getting medically ready for it!
As always, comments and questions are welcome. Also, if you like the article and feel your network might also, please share.
Kind regards,
Dr Dan Pronk.
Altamirano MP, KJ, Aden JK, Dubick MA 2015, ‘Role of the Windlass in Improvised Tourniquet Use on a Manikin Hemorrhage Model’, Journal of Special Operations Medicine, vol. 15, no. 2, pp. 42-46.
ANZCTC 2015, ‘Active Shooter Guidelines for Places of Mass Gathering’, viewed 8 December 2015,<http://www.nationalsecurity.gov.au/Media-and-publications/Publications/Documents/active-shooter-guidelines-places-mass-gathering.pdf%3E.
Australian Government 2018, Australian National Security National Terrorism Treat Advisory System, viewed 7 March 2018, <http://www.nationalsecurity.gov.au/Securityandyourcommunity/Pages/National-Terrorism-Threat-Advisory-System.aspx%3E.
Hirsch M, CP, Nizard R, et al. 2015, ‘The medical response to multisite terrorist attacks in Paris’, The Lancet,<http://www.thelancet.com/pb/assets/raw/Lancet/pdfs/S0140673615010636.pdf%3E.
Jacobs LM, WD, McSwain NE, Butler FK, Fabbri WP, Eastman AL, Rotondo M, Sinclair J, Burns KJ 2013, ‘The Hartford Consensus: THREAT, A Medical Disaster Preparedness Concept’, Journal of the American College of Surgeons, vol. 217, no. 5, pp. 947-953.
King DR, LA, Ramly EP, BostonTraumaCollaborative 2015, ‘Tourniquet use at the Boston Marathon bombing: Lost in translation’, The Journal of Trauma and Acute Care Surgery, vol. 78, no. 3, pp. 594-599.
LM, J 2015, ‘The Hartford Consensus III: Implementation of bleeding control’, Bulletin of The American College of Surgeons,<http://bulletin.facs.org/2015/07/the-hartford-consensus-iii-implementation-of-bleeding-control/%3E.
