This article focuses in on the tactical considerations of the Primary Survey that are applicable to first-responders in high-threat environments. Whilst it uses military examples to illustrate the points, the concepts are as just as applicable to civilian environments such as car crashes, animal attacks, fires or other natural disasters, and many other casualty situations where there is an ongoing potential danger of further casualties, or risk to the first-responder. In today’s political climate of transnational terror threat on the streets of first-world cities, these concepts are worth some consideration for any paramedic or other first-response provider.

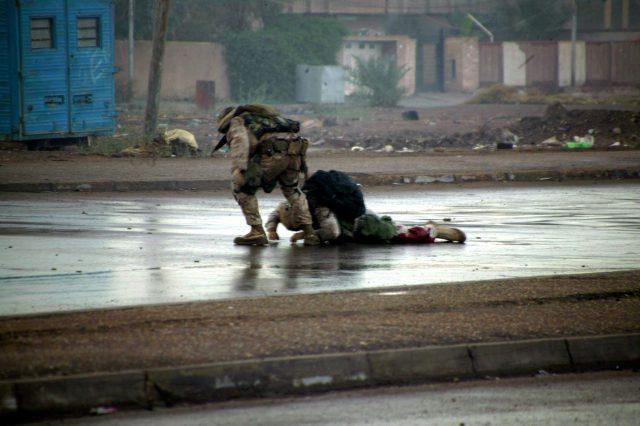
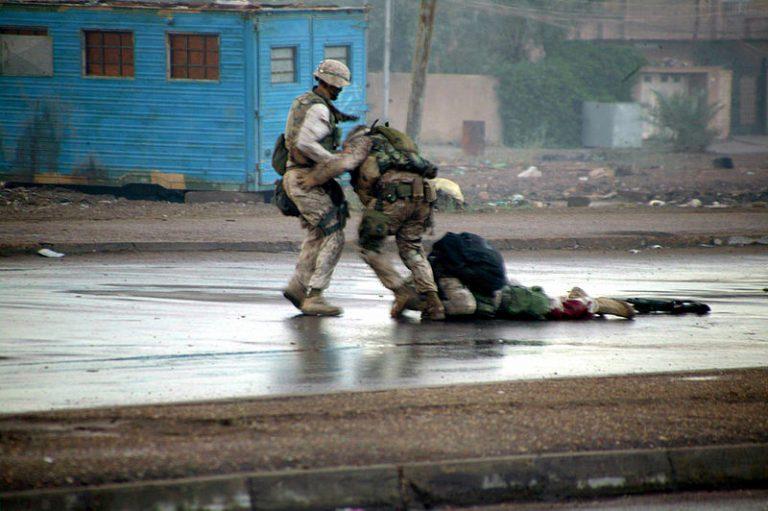
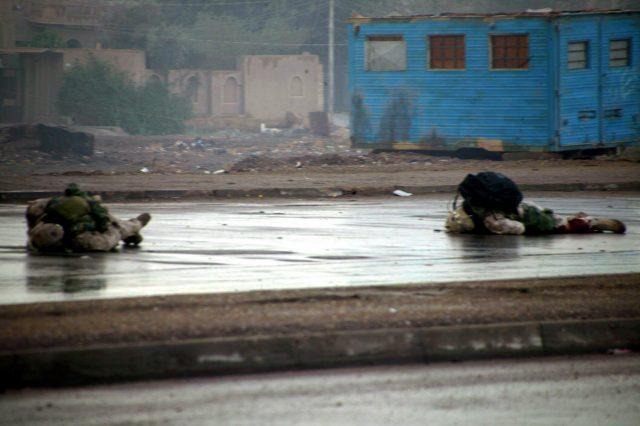
As first-responders it is inherent that we want to respond immediately to casualty situations. This is particularly the case in the instance of the military or law enforcement environment where the casualty may indeed be a teammate or close personal friend. Whilst this instinct is admirable it is important to be aware of, and train to have, the discipline to hold back on response for a brief period of time in order to properly assess the situation prior to engaging. Any student who has done even the most basic of first aid courses is likely to have been taught that the primary survey begins with a Danger assessment (Danger, Response, Airway, Breathing, Circulation). Whilst this is often well learned for the test on the day, it has been my experience that it can go out the window in the heat of the moment when the excitement of the situation takes over. The tendency to put the blinkers on and jump headlong into the situation is sometimes overwhelming, and I think most of us will confess to being guilty of it in the past, be it in training or the real scenario. For the most part in the hospital or civilian pre-hospital environment first-responders will get away with it, however in a high-threat casualty environment, it may prove costly. It is imperative in those environments that the first-responder take the time to properly assess the threat, and where possible minimise or eliminate it prior to engaging in their medical response. Whilst it may seem like an eternity as a casualty screams and bleeds whilst you assess the scene, those few moments may prove life saving. It may be that after a moment of consideration and threat assessment that the first-responder consciously choses to expose him or herself to the threat in order to help the casualties, and when this goes well it is the stuff of legends. When it goes poorly however, it can result in worsening of an already bad situation. One such graphic example of a casualty response turning to disaster occurred on the streets of Fallujah in November 2004 after a US Marine was downed by an enemy sniper. In an act of uncommon valor, a second marine, and then a third rushed out into the open to recover the initially casualty, both to be downed by the same enemy sniper, one killed, the other critically wounded. The situation was captured in a series of haunting images that serve as both a tribute to the brave men of the day, and a cautionary illustration of the need to asses for, and eliminate threats prior to engaging in casualty situations whenever possible.
Once the threat has been assessed, and where possible minimised or neutralised, and a decision has been made to engage in the casualty recovery and treatment, the next priority is to move safely to the casualty and recover them to a place of safety. Another option, if the casualty is conscious and able to, may be to stay in a place of safety yourself and yell at the casualty to crawl to you. Whilst in may seem intuitive for the casualty to want to move to safety, in the overwhelming situation of being injured and in pain, it may not have occurred to them, and all they may need is some prompting and direction from a first-responder.
It is often taught that you shouldn’t move a casualty for fear of worsening their injuries, particularly those who have suffered blunt force trauma such as car crashes or falls from height where spinal injuries are suspected. This is good advice in many instances, but must be evaluated in the context of the overall scenario. If the situation is safe and secure and you can leave the casualty in place to wait for assistance to arrive, then by all means minimise any unnecessary movement. If however the casualty or yourself are in harms way then the priority must be to move to a place of relative safety. An Ex-Special Forces friend of mine encountered this very situation when he was one of the first on scene at a civilian car crash in which a car had run an intersection and been struck by another car, spinning off and hitting a power pole. The driver of one car was unconscious in their seat and the overwhelming consensus from those first on scene was to leave her in place until the ambulance arrived. My friend, upon smelling fuel leaking from the car, promptly extricated the woman from the car and dragged her to a safe distance from the car in case it caught fire, much to the criticism of other bystanders. It was his assessment that the risk of the car exploding in flames outweighed the risk of an unstable cervical spine injury, and he chose to act. In my opinion he did the right thing.
Until the casualty has been recovered to a place of safety no medical assessments or interventions should be attempted. It may be appropriate to stop at the first place of relative safety to apply time-critical immediate life-saving interventions, such as arterial tourniquets, and then proceed to a secondary place of safety before doing a more comprehensive assessment and higher level interventions. The Committee on Tactical Combat Casualty Care (CoTCCC) refers to these immediate life-saving interventions as Care Under Fire (CUF), and whilst they are designed for use in combat, the principles can be adapted to civilian high-threat situations.
The following video demonstrates the principles discussed above in a military combat casualty training scenario. In the scenario a soldier has sustained a gunshot wound to the upper thigh resulting in a life-threatening arterial bleed, with an active enemy threat still in the area. The responding element assesses the situation without initially exposing themselves to the threat, and initially encourages the casualty to both apply their own tourniquet, and to crawl to cover. When these measures fail, a combination of covering fire and concealing smoke is used prior to swiftly recovering the casualty to a place of relative safety, before the casualty’s own arterial tourniquet is used to address the life-threatening haemorrhage and conserve the first-responder’s medical equipment for potential future requirement. As soon as the immediate life-threatening injury is addressed the recovery team extract the casualty to a place of higher safety prior to any further assessment or intervention.
It will be noted that in the video the DRABC acronym is not followed and the medical response goes straight from Danger and Response to Circulation, skipping Airway and Breathing along the way. In the military context, instead of the ABCs, the acronym MARCH, being Massive bleeding, Airway, Respirations, Circulation, and then Head injury / Hypothermia, is often adopted. This change in priorities is in recognition of bleeding out from compressible wounds being overwhelmingly the number one cause of preventable death on the battlefield (Beekley 2008; Bellamy 1984; Eastridge 2012; Kotwal 2011). Whilst these references relate to the military context, devices such as arterial tourniquets are being seen more and more in civilian first-response, in scenarios such as motor vehicle accidents, and more recently in response to terrorist mass casualty events on our streets, in which the wounding profiles of casualties are the same as those of war zones due to the use of Improvised Explosive Devices and assault rifles (Hirsch M 2015; King DR 2015).
Below is a video of an arterial tourniquet being applied by Police first-responders to a casualty with a traumatic leg amputation after being struck by a car.
A comprehensive introduction to Arterial Tourniquets for first-responders can be found in TacMed’s E-book titled “Arterial Tourniquets for Police Officers, Law Enforcement, and other First-Responders”, an overview of which including a free chapter can be found linked here.
Situational awareness is paramount in a tactical casualty response. Even once you have the casualty in a place of relative safety and have commenced your life-saving interventions, the tactical situation may deteriorate causing you to have to move locations again. This is an important consideration relating to how much of your medical kit you get out and spread around – always bear in mind the potential requirement to have to pack up quickly, and only get out the kit absolutely required for any given intervention. Another important factor which you need to remain situational aware of is how many casualties there are, and where they are all located. If you’re the highest trained medical asset on scene, there’s little point you tending to a relatively minor injured casualty when there might be a lesser medically trained person in the room next door struggling with a critically injured casualty. Ideally a Casualty Collection Point (CCP) is established, where all the casualties can be colocated, and in the optimal instance organised into areas according to the severity of their injury, or Triage category. There are various ways of allocating triage category, but in essence it relates to how badly injured a casualty is, and therefore the priority in which they need to be treated. If there are enough medical assets on the ground to tend to all casualties in a multiple casualty situation the scenario is termed a Multicas, and the most injured casualty is generally treated first. If the number or severity of casualties overwhelms the medical assets available then the situation is referred to as a MasCas and the concept of “reverse triage” may need to be applied. In this scenario, the most injured casualties who may require significant amounts of medical assets, and have little chance of survival, may be triaged as expectant and provided only basic medical interventions to try and preserve life, with the focus turned to slightly lesser injured casualties with a greater chance of survival with medical intervention. The goal in this setting is to provide the greatest good to the greatest number of casualties, rather than dedicating all your resources to a severely injured casualty with little chance of survival whilst two or three salvageable casualties may potentially die resultantly from lack of intervention. If more medical assets arrive, or all other casualties have been stabilised then attention might be turned back to helping the expectant casualties. The highest trained medical asset on scene should be the one allocating the triage category and maintaining scene oversight, as well as starting to document casualty information and thinking about evacuation priority. Ideally this scene commander should not get too bogged down in the management of individual casualties but should be available to plug in intermittently with casualty management for specialist interventions that may be above the skill level of the individual medical asset allocated to the casualty. As higher-level medical reinforcements arrive on scene, the scene command responsibility can be handed over to a higher authority as appropriate.
The following video shows a few minutes of a military multicas training scenario involving a simulated ambush in complex urban terrain. As discussed above, initial priority is on threat suppression / neutralisation, followed by safe movement of first-responders to the casualties, movement of the casualties to a place of relative safety, assessment of danger on the casualties, casualty colocation, situational awareness of the number of casualties and the ongoing tactical situation, adequate exposure of the casualties to assess wounds, immediate life-saving interventions, and informing higher authorities that the casualties have occurred.
The remainder of that training video unfortunately contained a few too many faces and names to be reproduced in this context, however it continued with an assessment of the casualty’s airway, respiration – including a log roll to assess for back exit wounds, and circulation assessment with bandaging of minor bleeders. Shortly after the above video finishes, further medical assets arrived on scene and I was able to hand my casualty over to one of my medics and assume the scene command role to gain situational awareness of all the casualties, and begin to collate information for detailed higher reporting as well as handover to the simulated AME medic who was inbound in the scenario to collect our casualties.
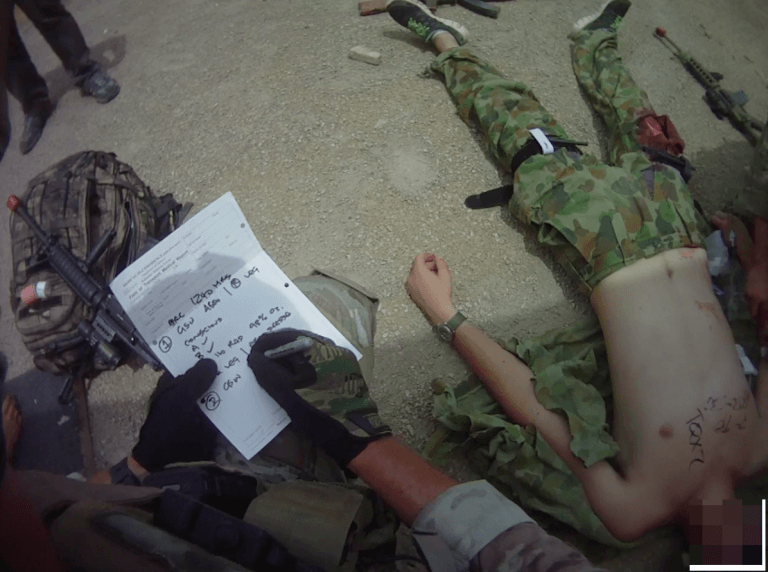
A few key points worth mentioning are illustrated by the still images from the video shown below:
In this image I’m using a pulse oximeter to gather vital information about my casualty. Whilst a relatively cheap and simple piece of equipment, the pulse oximeter is invaluable in the pre-hospital environment. Firstly, if the device is actually reading it tells me that the casualty is perfusing their peripheries, and has a systolic blood pressure >80 mmHg (approximately), and therefore is not in an advanced state of shock. The pulse rate, rhythm, and oxygen saturations can then be put together with the clinical appearance of the casualty to piece together the overall picture of how severely injured they are. If the oxygen saturations are reading lower than expected, it may prompt me to reassess the airway and breathing, including a detailed assessment of the casualty’s back if not already done. If the heart rate is higher than expected, it may alert me to occult internal bleeding, and indicate that the patient may be in shock. A rundown on the finer points of pulse oximeters and their use can be found at this previous TacMed Vlog. Worth being aware of is that casualties suffering from Carbon Monoxide poisoning may have an oxygen saturation reading of near 100% on pulse oximetry but may still be in desperate need of high-flow oxygen. This comes down to the basic pulse oximeter simply registering the saturation of the haemoglobin molecule, and not being able to differentiate whether the haemoglobin is saturated with oxygen or Carbon Monoxide. I’ve been caught out by this once! Also worth noting in the image is that my pulse oximeter is attached to me by a retractible lanyard, which can also be seen of my trauma shears in the Tactical Primary Survey video. In my experience, if these items weren’t physically attached to my person I would routinely lose them in the heat of a casualty situation.


In these images further medical assets have arrived, and as the highest medical authority on the scene I have handed over my casualty to another medic to continue treatment whilst I gain situational awareness of all the casualties and begin to document casualty cards for higher reporting and handover to the inbound AME team. Vital signs can be seen scribbled on the casualty’s chests by the treating medics. At all times my pack and rifle were kept within arms reach, with a minimum of kit spread around to allow for a rapid response to a new threat or a quick move if the tactical situation deteriorated.

Finally, whilst it is imperative to expose your casualty thoroughly to assess for wounds, once all immediate interventions have been attended to it is essential to cover them back up to keep them warm. As we all know, hypothermia is one of the three factors of the lethal triad, and along with acidosis and coagulopathy, will undo all the good work you’ve done for the casualty if you forget to rug them up and keep them warm for extraction.
Like all skills, those of the Tactical Primary Survey can only be mastered through repeated training, ideally in a Reality-Based Training (RBT) format. For more detail on the concept of RBT and how it applies to medical training please see TacMed’s previous post titled “Train as you’re going to fight: The importance of Reality Based Training” linked here. I also encourage anyone involved in training first-responders to have a read of the brilliant text “Training at the speed of life. The definitive textbook for military and law enforcement Reality Based Training” by Kenneth Murray (Murray 2006).
Whether it be in response to a traffic accident or a terrorist mass-casualty incident, in this day and age first-responders need to have an awareness of the tactical considerations as they apply to the Primary Survey. Being aware of, and training for, the contingencies discussed in this article may prove life saving not only for the casualties on the day, but potentially for the first-responder themselves.
Thanks for reading, as always comments and discussion are encouraged. If you feel others in your network might enjoy this article then please share it widely.
Kind regards, dan.
References
- Beekley, A, Sebesta, JA, Blackbourne, LH, et al. 2008, ’31st Combat Support Hospital Research Group. Prehospital tourniquet use in Operation Iraqi Freedom: effect on hemorrhage control and outcomes’, Journal of Trauma, vol. 64, pp. S28-S37.
- Bellamy, R 1984, ‘The causes of death in conventional land warfare: implications for combat casualty care research’, Military Medicine, vol. 149, no. 2, pp. 55-62.
- Eastridge, B, Mabry, RL, Seguin, P, Cantrell, J et al. 2012, ‘Death on the battlefield (2001Y2011): Implications for the future of combat casualty care’, Journal of Acute Care in Surgery, vol. 73, no. 6, pp. S431-S437.
- Hirsch M, C, Nizard R, et al. 2015, ‘The medical response to multisite terrorist attacks in Paris’, The Lancet,
- King DR, L, Ramly EP, BostonTraumaCollaborative 2015, ‘Tourniquet use at the Boston Marathon bombing: Lost in translation’, The Journal of Trauma and Acute Care Surgery, vol. 78, no. 3, pp. 594-599.
- Kotwal, R, Montgomery, HR, Kotwal, BM, Champion, HR, Butler, FK, Mabry, RL, Cain, JS, Blackbourne, LH, Mechler, KK, Holcomb, JB 2011, ‘Eliminating Preventable Death on the Battlefield’, Archives of Surgery, vol. 146, no. 12, pp. 1350-1358.
- Murray, K 2006, Training at the Speed of Life. The definitive textbook for military and law enforcement Reality Based Training, Armiger Publications, Gotha, FL.
