As I looked up from the bag of dismembered body parts in my hand I remember being slightly surprised by the expression of repulsion on the face of the experienced trauma surgeon standing next to me. His gaze moved from the severed arm I was holding to meet my eyes and he promptly confirmed that I had everything I needed before excusing himself and hastily leaving me and my fellow Special Forces medic to get back to the grisly task of trying to reassemble the dead bodies from the six bags of parts we had received. The blast that had ripped apart the members of our partner force’s bomb disposal crew had been a massive one, so much so that it was difficult to determine exactly how many bodies we actually had, it was either four or five. The coppery smell of blood, mixed with cordite, burned flesh and the purulent smell of spilled intestinal contents made the air in the resuscitation room dense and difficult to breathe without gagging. I found that breathing through my mouth helped a little. Our task was simple, to reunite the parts as best we could to the bodies they belonged to and then x-ray them all to ensure they were free from unexploded ordinance before they were to be flown back to their home villages for timely burial in accordance with local religious practices. I didn’t think much of it at the time, it wasn’t the first time I had handled multiple mutilated bodies and it would certainly not be the last. We completed the task to the best of our ability before having a quick shower and heading to dinner as usual and then to the pre-mission brief for the targeting operation the following day.
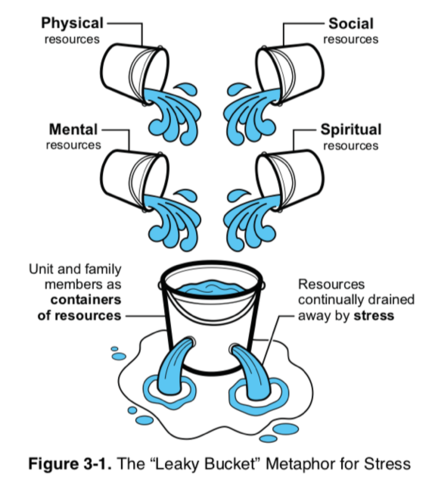
I caught up with the trauma surgeon about a week later and he mentioned the incident, apologising for his rapid exit from the resuscitation bay. The surgeon was a highly experienced veteran having started his career as a US Marine Corpsman in the Vietnam era and seeing active service in that conflict. He had then proceeded to become a doctor, then a surgeon and worked his way up the ranks to be in command of the main surgical facility in our Area of Operations at the time of the story above. He had witnessed more than his fair share of death and human suffering, and over a cup of coffee and a cigar he shared with me a powerful analogy of his relating to vicarious trauma and the bucket within all of us that eventually overflows if you don’t manage it well. It wasn’t until years later that I could even begin to appreciate the sage warning that the surgeon was giving me. In my mind at that time I was still bulletproof and still keen to be involved in every trauma I could, no matter if I was of any utility or not. To be brutally honest I loved it, the excitement and drama of death and near-death invigorated me, and I would walk away from touch-and-go resuscitations buzzing with energy no matter the outcome. Vicarious trauma was a drug of sorts and I was hooked. Like any drug of there are consequences of addiction and mine would come later. My bucket would eventually fill and overflow, and the significance of the surgeon’s words would come back to me only when it was too late.

Vicarious Trauma, as the name suggests, is trauma sustained by a person indirectly through exposure to traumatised individuals and traumatic events. Unsurprisingly it is high in occupations such as nurses, paramedics and medical staff, particularly in pre-hospital, mental health, military and Emergency Department environments, as well as in Police and Corrections Officers. When levels of Vicarious Trauma exceed the level of resilience of an exposed individual, that individual is prone to develop Secondary Traumatic Stress (STS). STS has symptoms parallel to those observed in persons directly exposed to trauma and near-identical to those seen in Post-Traumatic Stress Disorder (PTSD) including intrusive thoughts, tendency to avoid triggers, and hypervigilance (4). Similar to STS, Compassion Fatigue (CF) is another term now in common usage to describe the phenomenon of stress resulting from chronic exposure to traumatised individuals rather than from exposure to the trauma itself (2). CF is characterised by the following symptoms:
- Exhaustion
- Anger
- Irritability
- Negative coping behaviours such as alcohol and drug use
- Reduced ability to feel empathy and sympathy
- Diminished sense of enjoyment or satisfaction with work
- Increased absenteeism
- Impaired ability to make decisions and care for clients
I’m quite sure that anyone who has worked in any role dealing with traumatised individuals regularly will have experienced some or all of these symptoms or known someone who has. CF sufferers are likely to take their symptoms home with them resulting in a flow on effect on their family life as well as their work life. Ultimately chronic CF can lead to profound shifts in the way that helpers view the world and their loved ones (5).
From an organisational perspective CF can be equally as damaging resulting in (1):
- Decreased employee retention
- Increased use of sick days
- Decreased productivity
- Increased work-related errors
- Decreased employee engagement
- Significant avoidable costs for the organisation
From a physical health perspective, it has been demonstrated that those working in fast-paced, and especially relatively high-risk, occupations are prone to higher baseline states of autonomic “Fight or Flight” activation (6). (Linked here is a previous article I wrote on the body’s fight or flight system)
While this system can prime us well to deal with acute stress situations when activated chronically it can lead to a variety of stress-induced deleterious effects. A concerning study by McCraty & Atkinson (6) looking at Police Officers showed that the study cohort had significantly elevated autonomic arousal when compared to a control group, and 11% of the Officers studied had a risk of sudden cardiac death or other serious health challenge, representing a level twice that of the population average (6). Encouragingly the same study showed that stress levels, depression and negative emotions could be statistically significantly reduced with a concurrent improvement in work performance, teamwork and family relationships after the introduction of resilience training.
This introduces the elusive concept of resilience, which most of us are aware of but few of us have ever taken the time to really consider a true definition of the term. Indeed, opinion is divided in the literature as to whether resilience represents a characteristic of an individual or an outcome of a circumstance (7). What is generally accepted however is that resilience requires two factors, being a high-risk situation or threat and the successful adaptation to, or competence in, that situation (8). It is also recognised that resilience is a multidimensional construct which includes factors relating to individual attributes, family aspects, social environment, and culture (8).

What the evidence is now suggesting is that a proactive stance on building resilience and managing the cumulative trauma associated with roles in first-response and other professions high in vicarious trauma can have a profound impact on individual mental health and wellbeing, physical health, job satisfaction, as well as improvements in family life resulting from that trauma not being taken home and inadvertently inflicted second-hand on loved ones. While there is no cookie cutter one-size-fits-all approach to building resilience and managing work stress, a few ideas are offered below to get started.
Train as you’re going to fight
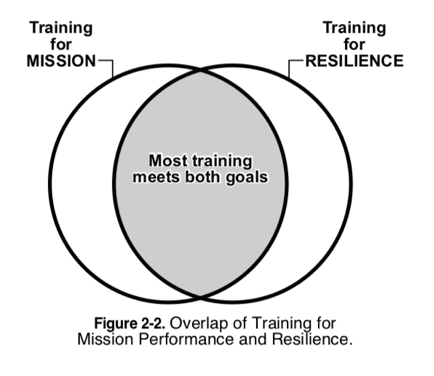
Anyone who has followed my previous work will know that I’m a massive advocate of Reality Based Training (RBT) and have seen first-hand the lifesaving results of skills programmed through high-fidelity training utilised in complex tactical trauma situations. Likewise, I have seen the devastating psychological sequalae of medical personnel who were unable to rise to the occasion when called upon due to a deficit in skill, perceived or otherwise, or an inability to appropriately perform a skill in a complex situation. In my opinion repeated high-fidelity RBT is the number one way to program these skills to be there in the moment of need, and training is logically a great way of building resilience to both specific situations that a first-responder may encounter, but also a broader resilience that comes from increased confidence in one’s own abilities. The United States Marine Corps illustrates this relationship eloquently in the following diagram taken from their outstanding Combat and Operational Stress Control manual (3).
Minimise work-related trauma
This one sounds relatively obvious but it’s surprising how many first-responders and emergency staff will voluntarily expose themselves to unnecessary workplace trauma. I was certainly guilty of exactly that in my early career when I would actively seek out involvement in any form of trauma resuscitation situation even when I was not contributing to the process in the slightest. To some degree I accept that there is a great learning opportunity in being a fly on the wall in a trauma situation, however as I progressed in my career I suspect my attendance in such unnecessary situations was more related to curiosity rather than learning opportunity. What resulted was a significant amount of unnecessary cumulative trauma exposure that contributed nothing to my individual learning or the patient outcome but did contribute over time to the filling of my personal bucket. I’m not suggesting that as a first-responder you should actively avoid trauma exposure as this is a fundamental part of the role and if you need to respond or assist in a situation then you must. What I’m suggesting is that if a situation is under control and your services are not required then in the long run it is probably better to walk away rather than engage in the situation and see yet another dying child or dead body. Likewise, if you are necessarily involved in a trauma situation and you have the ability to prevent other unnecessary people being exposed or involved then I would encourage you to actively do so. They may not appreciate being shut out of the situation at the time however long term I honestly believe that it is in their best interests. Throughout a career as a first-responder plenty of trauma will find you in your day-to-day work without actively seeking out unnecessary additional trauma.

Take stock of what’s on your plate
In this day and age of fast-paced connectivity it’s easy to get trapped on the treadmill of life running at ever-increasing speed. Over time the stresses in life accumulate one by one without us ever stopping to actively take stock of the demands on our time and energy. A simple stocktake of what’s on our plate can be a good start in building awareness of where stress is being added to our lives and could potentially be reduced or eliminated. As a part of this process it is also useful to assess your individual trauma inputs, some of which may not be as obvious as you think. For example, the constant low-level bombardment of negative news stories that we receive in our daily social media feeds, radio and television, and stories we hear, coupled with violent movies, TV shows, and first-person shooter computer games can potentially all add up to subliminally increasing our vicarious trauma levels. Many self-help gurus now advocate not following the news at all and to a significant degree I tend to agree with this stance on the rationale that if something important is happening in the world that I need to know about then I will be made aware of it while remaining able to insulate myself from horrible events happening halfway around the world that have no direct bearing on me and that I have no ability to influence. I appreciate that many will view this technique as ignorant and argue that a working knowledge of current affairs is essential to social interaction and that’s fair – I simply offer this as one of many potential strategies for consideration to reduce unnecessary cumulative vicarious trauma.
Practice mindfulness and meditation
If someone had have told me ten years ago that I would be practicing mindfulness and meditation on a daily basis I would have been at very real risk of laughing directly in their face! The truth is that I wasn’t ready to hear that back then but with hindsight I wish I had have been. I have found the simple act of disciplining the mind to be calm and present even for short periods of time each day has led to a huge improvement to my ability to keep perspective on the world around me and control my impulsive responses to situations that would have previously elicited a hair-trigger reaction. I have come to think of the ability to practice mindfulness as akin to the safety switch on an assault rifle, allowing the selection of a semiautomatic response with deliberately chosen individual shots in response to a stimulus as opposed to selecting fully automatic and spraying out less considered responses without proper aim. There are no shortage of apps available these days for guided mindfulness and meditation practices and I encourage anyone reading, especially the manly men out there, to consider downloading one and giving it a try.
Exercise
There is an abundance of literature out there relating to the benefits of exercise on physical health and psychological wellbeing, and it is outside the scope of this article to delve into the detail. Purists will argue back and forth about the specific benefits of different types of exercise and how many sessions are required a week to maximise benefits, but in my opinion just getting out and doing something is the key here even if it is as simple as walking the dog or going for a dip at the beach.
Have a transition between work and home
This technique is key in not inadvertently taking work home with you and dumping it on your family and loved ones leading to the potential flow-on impact of damaging those relationships. The simple practice of taking stock of how you are feeling when leaving the workplace is a great start, followed by looking at ways to create a transition between work and home, be it mental or physical or both. Techniques that have worked for me include stopping at the gym on the way home to decompress and get an endorphin hit before arriving home after a stressful day, riding my bike or running to and from work to achieve the same, or listening to an audiobook during my commute home from work. Coupled to this I find it useful to take a mindful minute or two on reaching my home but before going in to consider the person I need to be when I walk through the door. This simple process allows me to consciously recalibrate to be the best version of myself to greet my wife and kids rather than the frustrated and angry version of myself that may have left the office that day.
Be aware of maladaptive coping strategies
The problem with maladaptive coping strategies is that they do actually work in the short-term to relieve symptoms which often serves to reinforce the behaviour, however in the long-term they are profoundly counterproductive. Alcohol is good example of a maladaptive coping strategy that most will be familiar with, and I suspect many readers will have had a bad day at work once in a while and gone home and had a few drinks to decompress and forget the day. The problem with that plan is that work is still there the next day and you need to face it with a hangover, and it can easily be seen how this scenario can quickly become a downward spiral. Other maladaptive coping strategies include anxious avoidance – where we actively avoid situations that we know are likely to cause us stress, thus never facing them and developing more adaptive coping mechanisms to deal with the situation, and sensitising where we learn, rehearse and anticipate fearful events leading to hypervigilance and excessive worrying. The latter response is designed to prime you for an encounter where you may need to respond to stress, however if chronically activated leads to a near constant state of anxiety and stress hormone response regarding events that are yet to happen and most likely never will.
The goal of this article is to raise awareness of the very real exposure to vicarious trauma among first-responders and related occupations, and to outline some of the symptoms of its sequalae and provide a handful of potential strategies to mitigate the compounding impact of trauma over a career. It is my hope that it will reach people in high-risk occupations and pique an interest in further study into the topics discussed and potential implementation of strategies before their buckets begin to fill and overflow. In conclusion I would like to leave you with another bucket analogy, once again taken from the United States Marine Corps Combat and Operational Stress Control manual (3), that I feel illustrates nicely the state of flux that our stress systems are under depending on how fast they are leaking versus how much we are replenishing them.
As always questions, comments and criticisms are welcome. Cheers, dan (LinkedIn)
Reference List
- Adimando, A (2018) Preventing and Alleviating Compassion Fatigue Through Self-Care. Journal of Holistic Nursing. 36(4): 304-17.
- Cocker & Joss (2016). Compassion Fatigue among Helathcare, Emergency and Community Service Workers: A systematic Review. Int. J. Environ. Res. Public Health. 13(618): 1-18
- Department of The Navy (2010): US Marine Corps Combat and Operational Stress Control. https://www.doctrine.usmc.mil
- Malkina-Pykh, IG (2017). Associations of Burnout, Secondary Traumatic Stress and Individual Differences among Correctional Psychologists. Journal of Forensic Science and Research. 1: 18-34.
- Mathhieu, F (2017) Transforming Compassion Fatigue into Compassion Satisfaction: Top 12 self-care tips for helpers. Workshop for helping professionals. 2017 Jail Healthcare Conference
- McCraty & Atkinson (2012) Resilience Training Program Reduces Physiological and Psychological Stress in Police Officers. Global Advances in Health and Medicine. 1 (5): 44-66.
- Pooley et al. (2010) Resilience: A Definition in Context. The Australian Community Psychologist. 22 (1): 30-37
- Ungar, M (2008). Resilience across cultures. The British Journal of Social Work, 38 218-235
